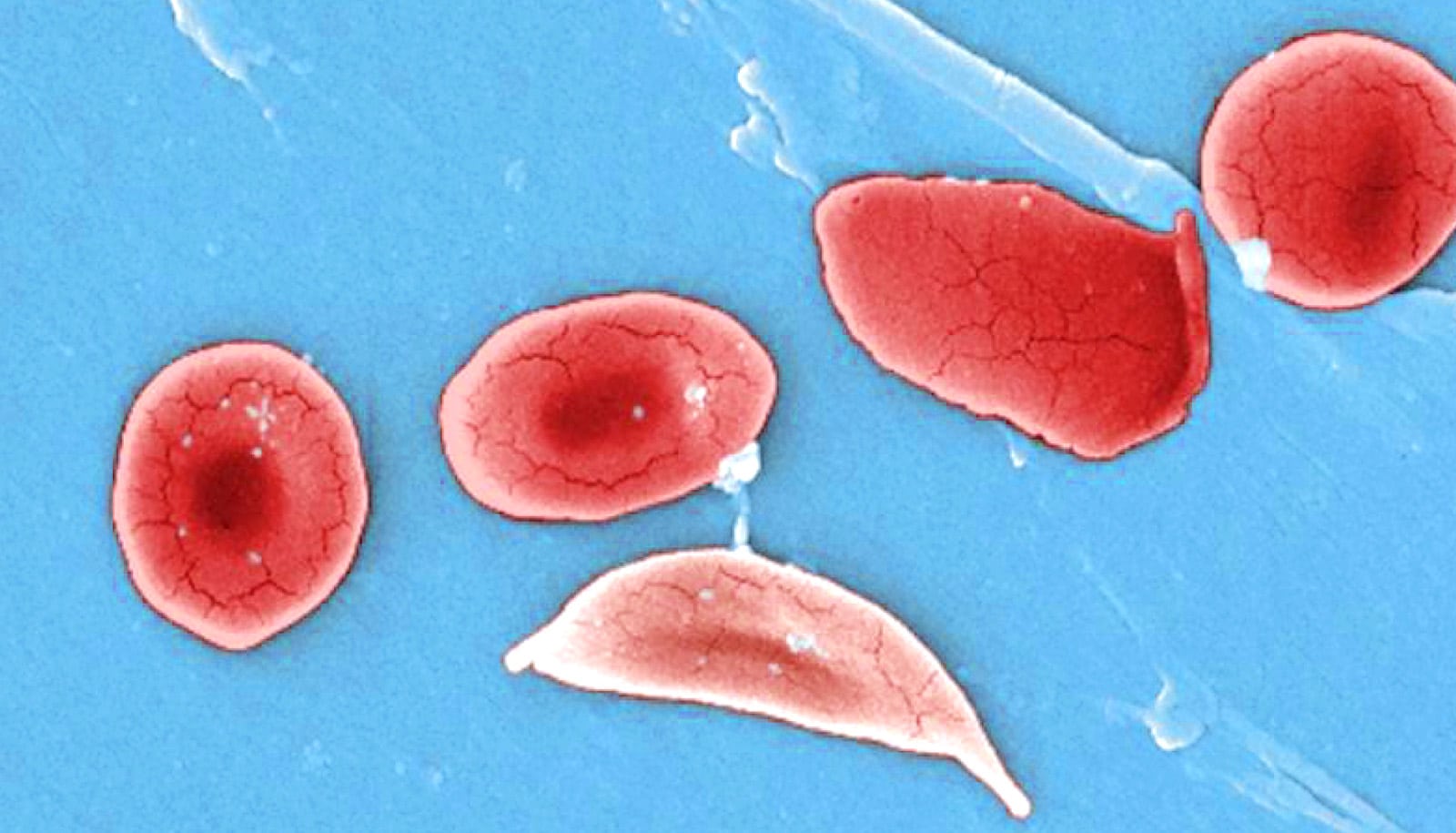
A new gene-editing approach could offer new hope to people with sickle cell disease.
Current gene therapies to treat sickle cell disease are complex, time-consuming, and are sometimes linked to serious side effects like infertility or blood cancer.
To address these challenges, researchers have developed special nanoparticles that can send gene treatment directly to various types of cells in bone marrow to correct the disease-causing mutations.
“This gene editing approach would allow patients to receive the medicine through a transfusion,” says study lead author Xizhen Lian, an assistant research scientist affiliated with the Johns Hopkins Whiting School of Engineering’s Institute for NanoBioTechnology and the Johns Hopkins School of Medicine.
“This avoids the lengthy, difficult process of many current gene therapies, decreasing the burden on patients and the health care system while minimizing treatment side effects.”
Their results appear in Nature Nanotechnology.
The research team, which included scientists at the University of Texas Southwestern Medical Center, St. Jude Children’s Research Hospital, Harvard University, and Johns Hopkins School of Medicine, used CRISPR/Cas and base gene-editing techniques in a mouse model of sickle cell disease to activate a form of hemoglobin and correct the sickle cell mutation. The team also found the approach effective in targeting leukemia cells.
“One challenge we encountered is that the stem cell population is very small; only 0.1% of cells in bone marrow are stem cells. They are also protected in a micro-environment that can prevent the delivery of drugs from circulation,” Lian says.
The team solved this problem by adding a special fat molecule into their tiny delivery particles. This new molecule helped the delivery particles find and strongly attach to the stem cells, delivering important gene therapy.
The team’s next step is to optimize this technology on a humanized animal model that can better mimic clinical scenarios, as they are currently working solely with rodent blood cells and components. Humanized animal models have been genetically modified to express human genes, cells, and proteins, allowing researchers to study human diseases in a living system that closely resembles that of humans.
“Our approach promises to help patients avoid invasive treatment procedures, which will significantly reduce the side effects of blood cancer because there is no random gene insertion into the patient’s genes. We are targeting a specific gene that causes the disease and that’s it,” Lian says.
“The only way to cure such genetic diseases is to correct the genetic mutation in the stem cell populations.”
Source: Johnny Moseman for Johns Hopkins University
Author Profile
- "Center" Bias Rating
- Futurity is a nonprofit website that aggregates news articles about scientific research conducted at prominent universities in the United States, the United Kingdom, Canada, Europe, Asia, and Australia. It is hosted and edited by the University of Rochester.
Latest entries
 ScienceSeptember 6, 2024Experts warn of rise in kids having sugary drinks
ScienceSeptember 6, 2024Experts warn of rise in kids having sugary drinks ScienceSeptember 6, 2024Watch a tiny bug do the world’s fastest backflip
ScienceSeptember 6, 2024Watch a tiny bug do the world’s fastest backflip ScienceSeptember 5, 2024TB discovery may upend ideas about the immune system
ScienceSeptember 5, 2024TB discovery may upend ideas about the immune system ScienceSeptember 5, 2024There’s a big disconnect between beef eaters and pollution
ScienceSeptember 5, 2024There’s a big disconnect between beef eaters and pollution