Politics, Policy, Political News Top Stories
The lack of specialized Covid-19 treatments for people with weak immune systems has left millions of Americans with limited options if they get sick as the pandemic heads into an uncertain winter.
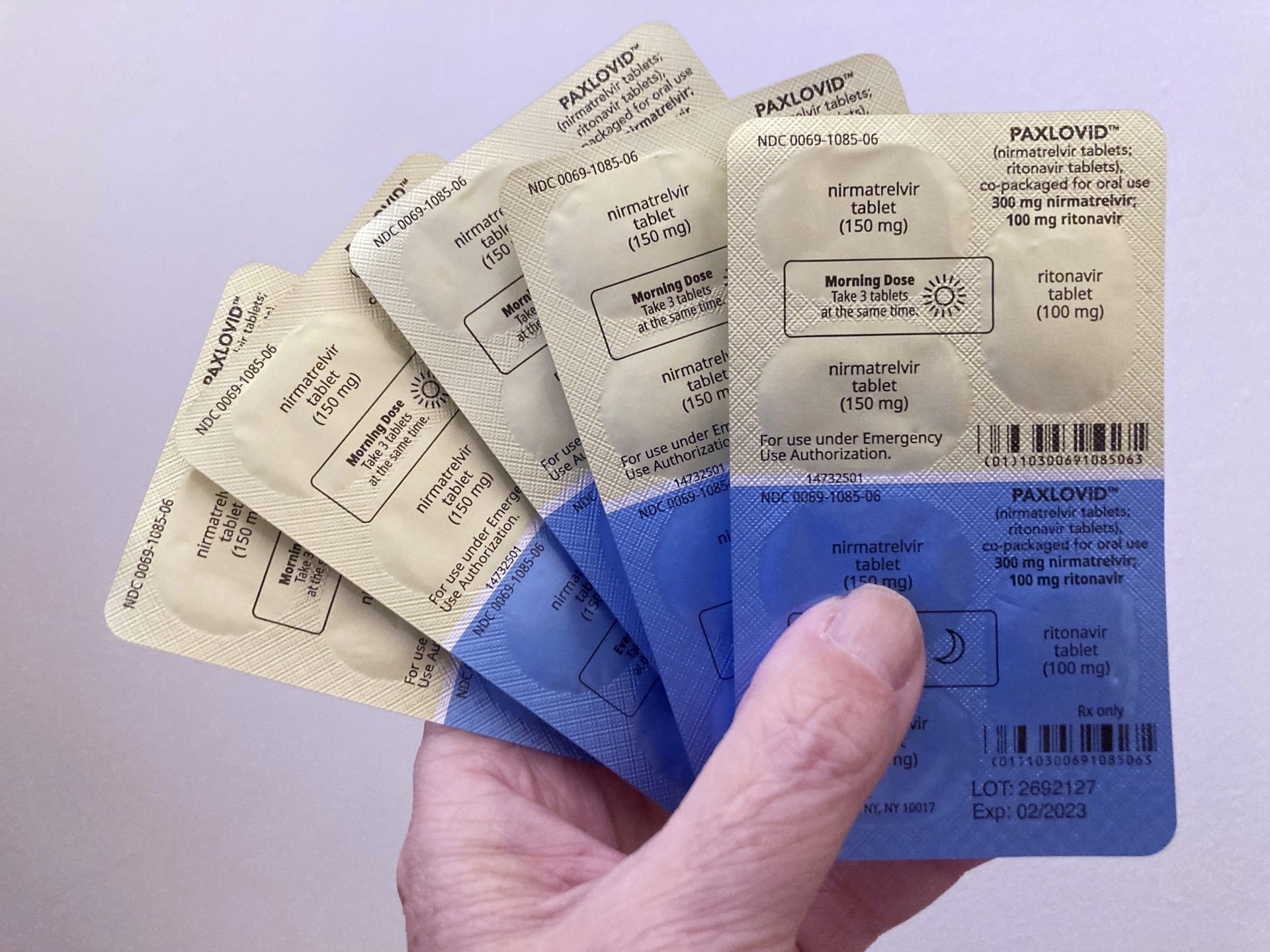
Once heralded as game-changers for Covid patients considered at risk for getting seriously ill — one was used to treat then-President Donald Trump in 2020 — monoclonal antibodies are now largely ineffective against current Covid variants. Easier-to-administer antiviral drugs, such as Paxlovid, have largely taken their place but aren’t safe for all immune-compromised people because they interact with many other drugs.
But the federal government funding that drove drug development in the early days of the pandemic has dried up, and lawmakers have rebuffed the Biden administration’s pleas for more. Without that, there’s little incentive for drugmakers to work on new antibody treatments that could be more effective.
And without a government program like Operation Warp Speed to develop second-generation vaccines and treatments, at-risk patients could be in danger of developing severe cases of Covid and flooding hospitals when the U.S. health care system is already strained, thanks to an influx of patients with an array of respiratory illnesses, including flu and RSV.
“Just because we have exited the emergency phase of the pandemic does not mean that Covid is over or that it no longer poses a danger,” said Leana Wen, a public health professor at George Washington University and former Baltimore health commissioner. “There are millions of Americans who are vulnerable to severe illness.”
The FDA pulled authorizations for four antibody treatments in 2022 as Omicron and its myriad subvariants wiped out their effectiveness. The treatments were geared toward adult and pediatric patients with mild-to-moderate Covid who were considered at risk of developing severe disease and ending up hospitalized.
While antiviral pills are plentiful and remain an option for some with weak immune systems, they won’t work for everyone — Pfizer’s Paxlovid interacts with many widely prescribed drugs.
Monoclonal antibodies — which have been made by companies like Regeneron, Eli Lilly and Vir — are lab-created molecules designed to block a virus’ entry into human cells. But they must bind to the virus’ spike protein to neutralize it, and the coronavirus’ many mutations since its 2019 emergence have gradually rendered the available products ineffective.
“It’s a bit risky to develop this,” said Arturo Casadevall of the Johns Hopkins Bloomberg School of Public Health, pointing to how quickly some Covid variants have surfaced before quickly receding.
A massive spending bill that lawmakers passed before Christmas left out the administration’s $9 billion request for more money to fight the pandemic, meaning there are fewer dollars to be spread around to address emerging Covid needs.
“Due to congressional inaction and a lack of funding, HHS does not have the resources it needs to fund the development of new treatments, and we could find ourselves with a very limited medicine cabinet at a time when we need more tools to combat Covid-19,” a department spokesperson told POLITICO, adding that HHS is working with providers and other groups “to ensure that Americans are able to take advantage of all available treatment options.”
The Biden administration has strongly promoted oral antiviral regimens like Paxlovid, which debuted a year ago and marked a turning point in managing the virus for most Americans.
Immunocompromised individuals — who are either born with immune-suppressing conditions or acquire them after organ transplants or by taking certain drugs — also may not mount sufficient immune responses after vaccination, making treatment options like antibody therapies a critical tool for them.
A CDC alert issued Dec. 20 to clinicians and public health professionals warned of the lack of viable monoclonal antibody treatments — including the diminished efficacy of a prophylactic antibody, Evusheld — and the availability of the antiviral options that to date have seen lackluster uptake. The agency urged providers to consult the National Institutes of Health’s Covid treatment guidelines for ways to potentially manage drug interactions with Paxlovid, such as temporary pauses or reductions in dose.
Remdesivir, an antiviral administered intravenously, is another treatment option for the immunocompromised, but it requires infusions over three days in either hospital or outpatient settings. HHS is urging states to support its health departments and systems in setting up infusion clinics to expand access to remdesivir, especially on an outpatient basis, and is working with maker Gilead to broaden the types of providers eligible to buy the drug.
Covid convalescent plasma remains an option for immunocompromised people who contract the virus, but its availability is scattershot across the country, Casadevall said. The treatment has pros and cons, he said — it’s less likely to be defeated by any one variant and can adapt to different strains, but it’s difficult to administer and requires blood-typing to be done for the recipient.
Still, Casadevall said, the main issue is educational because its use has changed since the pandemic’s early days, when treatments were scarce. Some hospital systems, like Hopkins, use it routinely, while some doctors don’t know plasma is still an option, he said.
The FDA has authorized the emergency use of convalescent plasma containing high Covid antibody levels for immunocompromised patients. But NIH has remained neutral on the treatment in that population, which Janet Handal, president of the Transplant Recipients and Immunocompromised Patient Advocacy Group, says has led to some hospitals balking at administering it.
NIH spokesperson Renate Myles pointed to the agency’s treatment guidelines for Covid, which are developed by an expert panel.
The recommendations for Covid convalescent plasma, last updated on Dec. 1, say there’s “insufficient evidence” to recommend for or against the treatment’s use in immunocompromised patients, while noting some panel members would use plasma to treat an immunocompromised person “with significant symptoms attributable to COVID-19 and with signs of active [viral] replication and who is having an inadequate response to available therapies.”
“In these cases, clinicians should attempt to obtain high-titer [Covid convalescent plasma] from a vaccinated donor who recently recovered from Covid-19 likely caused by a … variant similar to the variant causing the patient’s illness,” the guidelines say.
Casadevall, who leads the Covid-19 Convalescent Plasma Project, says NIH’s stance on plasma is inconsistent with its previous recommendations of monoclonal antibodies, which were made without clinical efficacy data, since Covid antibodies are the active component in both therapies. He led a petition earlier this month — signed by several doctors, including past and current presidents of the Infectious Diseases Society of America — asking NIH to change its recommendations.
Handal’s group also has asked the NIH and the White House to convene a meeting with scientists on the issue.
“To just not be having a dialogue about it is infuriating to us,” Handal said. “People are dying while people are just going through this bureaucratic dance.”
The FDA and European Medicines Agency held a virtual workshop this month to bring doctors, industry and regulators together to discuss supporting novel monoclonal antibody treatments.
“The FDA is committed to working with industry sponsors to expedite the development of new drug products to meet unmet needs, such as the need for new preventive therapies for immune-suppressed patients who are unlikely to respond to vaccination,” an agency spokesperson said.
In the meantime, Regeneron spokesperson Tammy Allen said the company, whose antibody cocktail’s use was limited in January, is committed to evaluating antibody treatment options as the coronavirus evolves.
“We believe monoclonal antibodies have played an important role in the COVID-19 pandemic to date and may again in the future, particularly among people with immunocompromising conditions,” Allen said.
Vir, which partnered with GSK on sotrovimab, continues to study whether the treatment could work against emerging variants and is also evaluating next-generation antibodies and small-molecule therapies, said spokesperson Carly Scaduto.
Still, pharmaceutical companies may be more inclined — both financially and practically — to pursue developing better antiviral pills that pose fewer drug interactions and are easier to administer, said Jason Gallagher, a clinical pharmacy specialist in infectious diseases at Temple University Hospital. Antivirals also hold up better against an ever-changing virus, he added.
“There’s way more money in Paxlovid than there is in any monoclonal” antibody treatment, Gallagher said, and it may take incentives to drugmakers to encourage their development. “They’re not going to make anyone really rich.”